Healthcare Case Studies
Case Study:
Healthcare Predictive Analytics: Right Care for the Right People
Goal:
A healthcare insurance company sought to boost member enrollment in its care management programs to reach the members with the highest needs, meet federal contract enrollment requirements, and ultimately improve health conditions and outcomes for its high-risk members.
Solution:
Our program consultant led a team of clinicians, IT professionals, and analytics experts to design and implement analytics models with data pipelines that stratified individuals according to health risks and behavioral profiles. Using a population of 318,000 members, the risk stratification models identified and prioritized members for care programs based on their health risks and likelihood of engagement. These members were then added to clinicians' work queues for potential enrollment and outreach.
Results:
Program enrollment for the clinical team significantly increased and exceeded contract targets for the year, resulting in incentive payouts for the healthcare insurance company.
Equally important, clinicians reported greater efficacy in member engagement, care planning, and interventions aimed at improving management of care, individual health conditions, and outcomes. Additionally, the project team was recognized for its program success and innovative approach.

Case Study:
Improving Healthcare Efficiencies and Cost of Care with AI
Challenge:
Clients for a healthcare insurance company demanded reductions in their insurance costs without compromising care quality and outcomes for covered employees.
Traditional Approach:
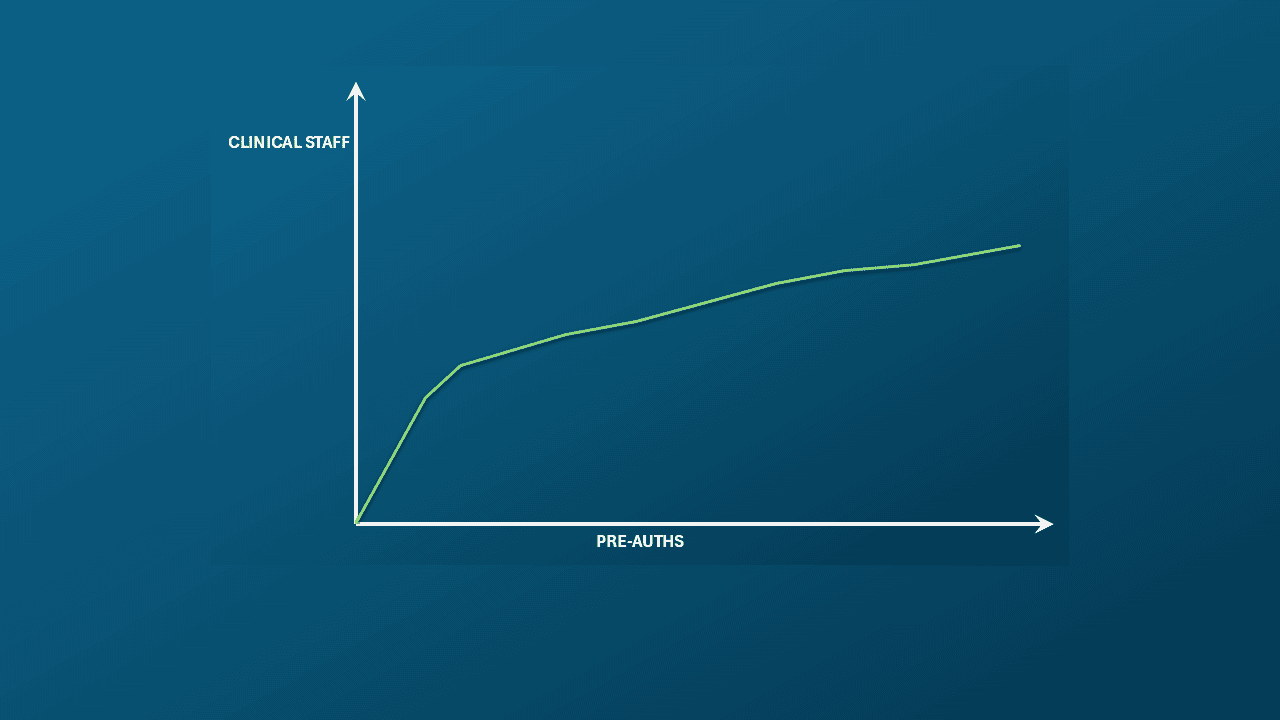
Healthcare insurers typically use more pre-authorizations to limit unnecessary medical use and manage costs, but this increases demand for clinicians and in turn raises costs. The direct correlation between the use of pre-authorization and costs was a real problem for this health insurers as noted in the chart.
Solution:
A proof of concept was conducted to develop a custom AI solution that applies natural language processing (NLP) and machine learning to improve medical records reviews and pre-authorization recommendations. The approach utilized a “human-in-the-loop” process, with licensed clinicians validating responses, and making all care decisions. The solution included explainability features to clarify how and why recommendations were generated and enabling clinicians to provide feedback for model improvement. Additionally, checks and balances were integrated into the workflow review process to maintain compliance with industry managed care guidelines, regulations, and standards.
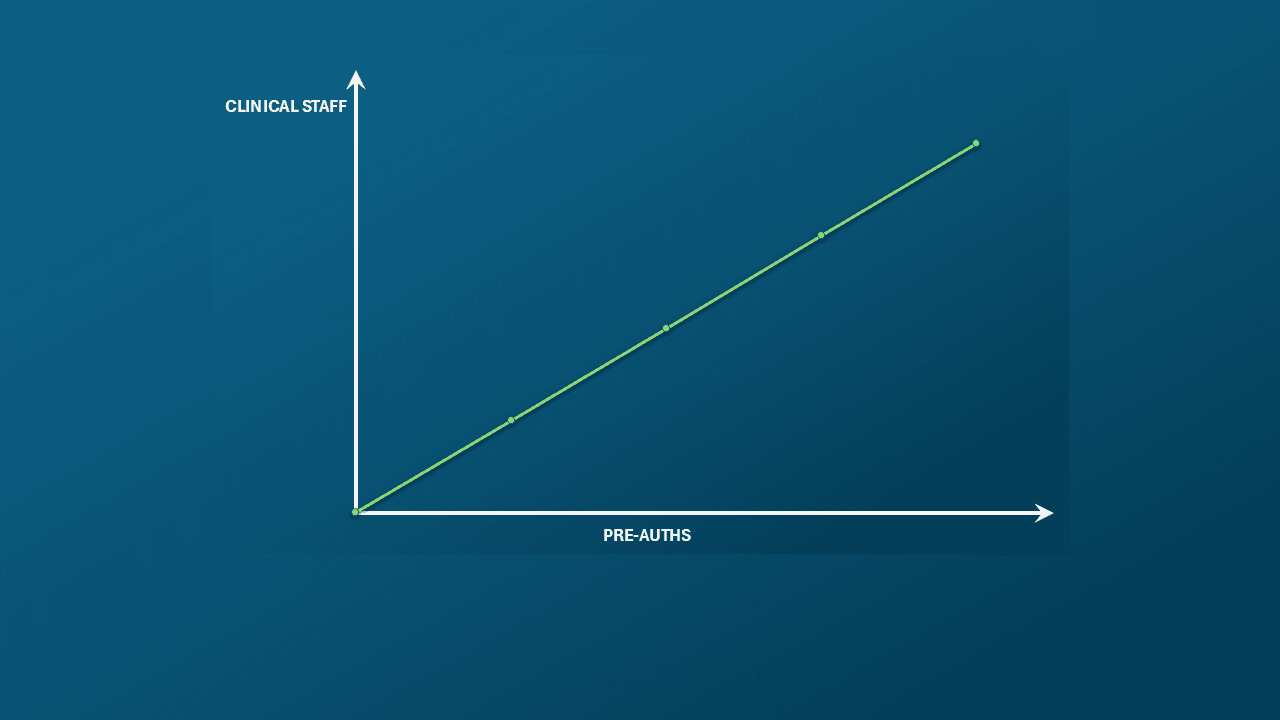
Results - "Bent the Curve"
The POC “bent the curve”, changing the relationship between auth volume and staffing requirements, enabling a new capability to "do more with existing staff”. Additionally benefits realized:
- Increased clinical staff efficiency by 27%, reduced administrative costs, and decreased inconsistencies and errors in medical reviews
- Helped clinicians to effectively manage caseloads, reduce administrative burden, & maintain comply care guidelines
- Approval of a multi-million, multi-year technology investment with an estimated ROI of 46% once scaled